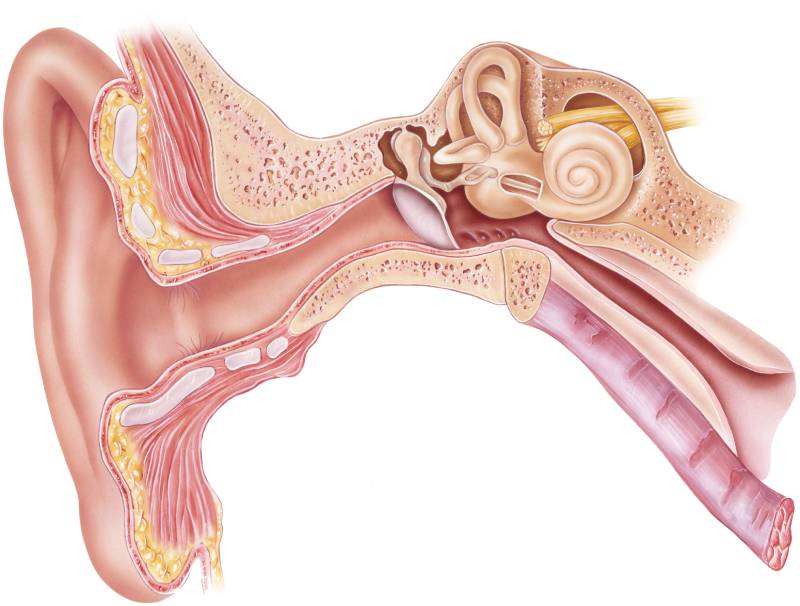
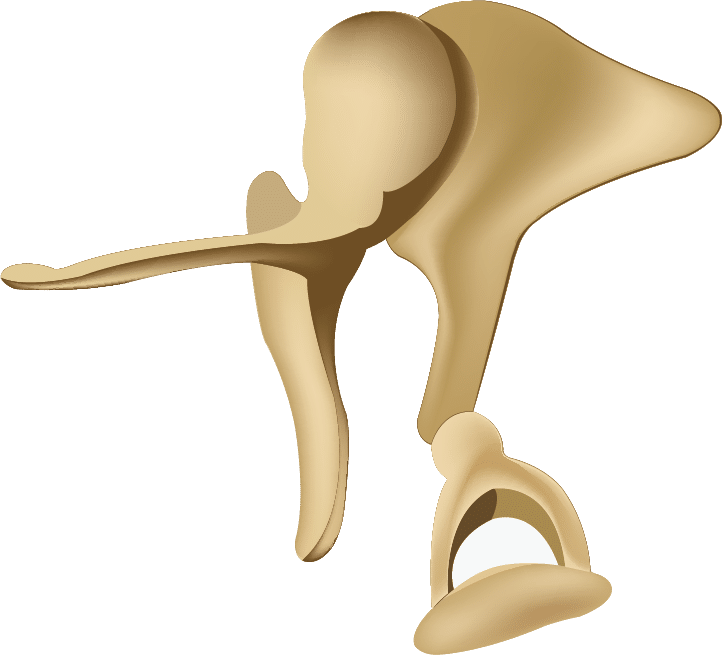
The temporal bone is divided functionally into the outer ear, middle ear, and inner ear (Figure 1). As sound enters the ear, it travels through the external auditory canal, vibrates the tympanic membrane and middle ear bones (also called ossicles) (Figure 2), and then is translated into a neural impulse by the inner ear. As we tour the temporal bone, we will follow the course of received sound and discover which otologic and neurotologic disorders can disrupt the process of hearing.
Outer Ear

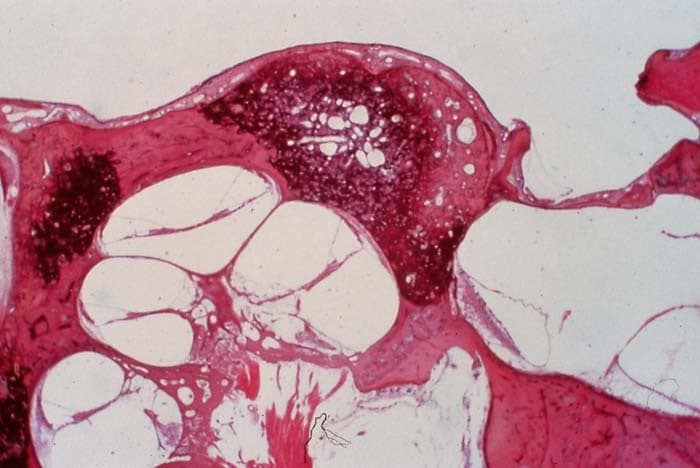
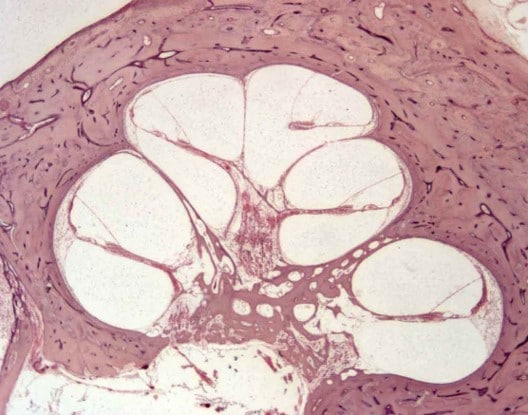
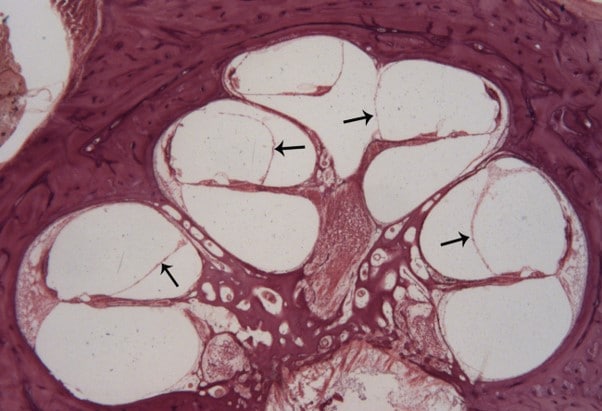
The external auditory canal (EAC) is about 2.5 cm long and is made of bone (2/3) and cartilage (1/3). Common causes of EAC obstruction are cerumen (ear wax), infection (also called otitis externa or swimmer’s ear), foreign bodies, and growths. Cerumen is produced by modified sweat glands in the EAC and serves as a protective function against infection. One of the most common disorders of the EAC in Southern California is bony growths caused by cold water and evaporation in the ear canal—also called exostoses or surfer’s ear (Figure 3).
Middle Ear

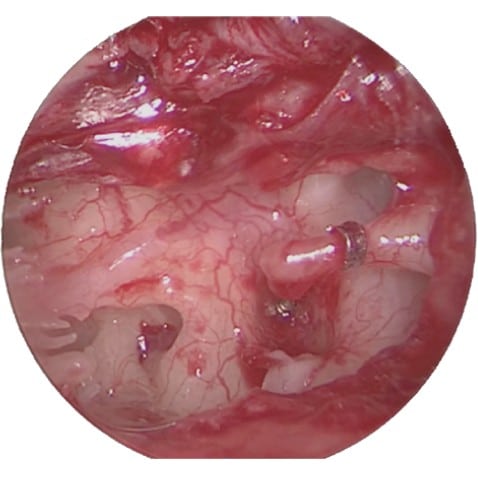
The middle ear extends from the tympanic membrane (TM) through an air-filled space to the oval and round windows into the inner ear. The TM (Figure 4) can be disrupted by infection (or Q-tips) and may require tympanoplasty (surgical repair). The old adage that nothing smaller than your elbow should go in your ear is true!
The middle ear space contains the ossicles (middle ear bones), which have a transformer mechanism that amplifies sound 22:1. Sometimes these bones are affected by infection or ingrowth of skin (cholesteatoma) and may need to be replaced. The stapes, which is the smallest bone in the body, is often replaced in patients with otosclerosis, a temporal bone disorder that causes the stapes to become fixed and stop vibrating (Figures 5-7).

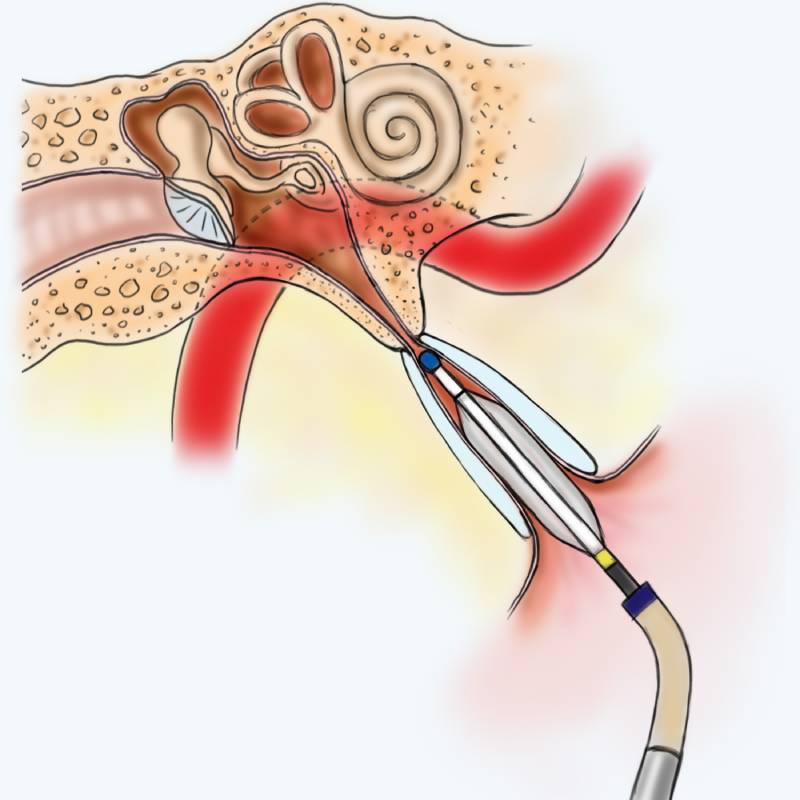
The Eustachian tube (ET) equalizes the pressure of the middle ear space by its communication with the back of the nasal cavity (nasopharynx). When the ET does not open and close well, patients can have ear pressure, middle ear fluid, and problems with the eardrum. Eustachian balloon tuboplasty is a relatively new surgical procedure that dilates the ET to improve its function (Figure 8).
Inner Ear
As the base (or footplate) of the stapes vibrates, it causes a movement of fluid inside of the cochlea. Shearing forces between the tips of inner hair cells and a membrane in the Organ of Corti translate this energy into a neural impulse, which travels along the cochlear nerve to ultimately reach the hearing centers in the brain. In addition to the cochlea, the inner ear consists of the balance organs (semicircular canals, utricle, and saccule). One disease process that can affect all parts of the inner ear is Meniere’s Disease. This disorder causes hearing loss, tinnitus, ear fullness, and vertigo and is associated with extra fluid inside the cochlea (or endolymphatic hydrops) (Figure 9).

When nerve hearing is lost, hearing aids can amplify sound to help patients hear better, but hearing aids are not effective for severe to profound hearing loss. The cochlear implant, first developed at the House Clinic, is an implantable device that can restore hearing to these patients (Figure 10). This remarkable technology filters the incoming sound into frequency bands and directly stimulates the cochlear nerve through an electrode placed inside of the cochlea.
The hearing and balance nerve (or cochlear and vestibular nerves) can also be affected by a benign growth called a vestibular schwannoma (also known as VS or acoustic neuroma). These tumors usually grow slowly and can affect hearing and balance. The House Clinic revolutionized microsurgical treatment for VS and is at the cutting edge of VS research and treatment today.